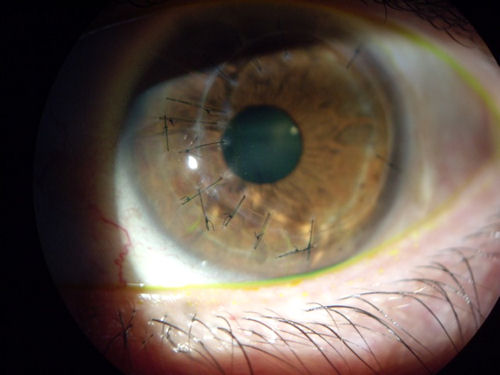
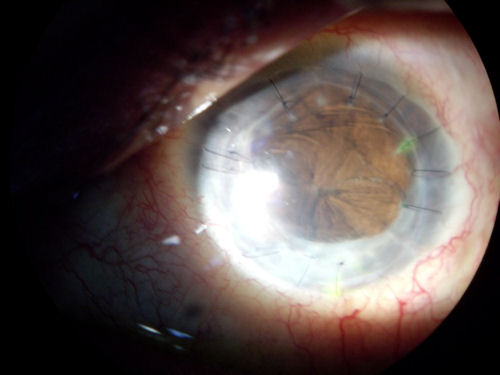
The photo below shows the cornea of a patient who had RK (radial keratotomy) surgery in 1988. Eighteen years later she developed an infection and inflammation. In all likelihood, an opportunistic organism penetrated the cornea through an RK incision. The infection was unresponsive to antibiotic eye drops; therefore, the patient was hospitalized and treated with a 7-day course of intravenous antibiotics. Unfortunately, the damage to the cornea led to need for a corneal transplant. Due to large open RK incisions, scar tissue from infection, and the extremely irregular corneal surface, the surgeon was forced to place the donor cornea off-center. The vertically placed sutures located at 9:00 and 7:00 were placed to prevent the open RK incisions from rupturing.
The 2nd image is the same eye two years earlier, post corneal transplant, with stitches holding the decentered donor tissue in place.

 Below is a photo of an eye blinded as a result of a corneal transplant gone bad.
Below is a photo of an eye blinded as a result of a corneal transplant gone bad. 
The photo below is a rejected corneal transplant. The patient had four previous corneal transplants.
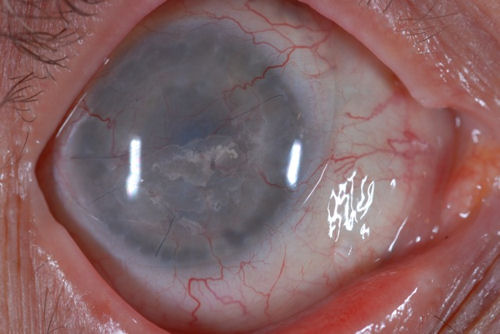


The patient is now blind in this eye with no light perception and no possibility of regaining useful vision. We published this patient's case to make the point that a corneal transplant is not a risk free procedure. Although what you see here is extremely rare, there is always the unforeseeable that may occur when any type of invasive eye surgery is undertaken.
July 2009 update: This patient has developed severe eye infection and inflammation and will probably have to have the eye removed due to recurrent infections and constant pain. These images are being published to warn patients that unexpected complications can take place with disastrous consequences. When it comes to the eye, nothing should be taken for granted.


The photo below is of a rejected corneal transplant.


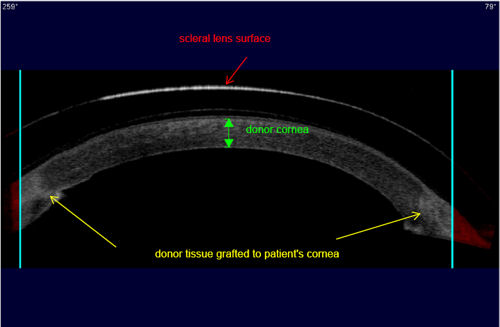
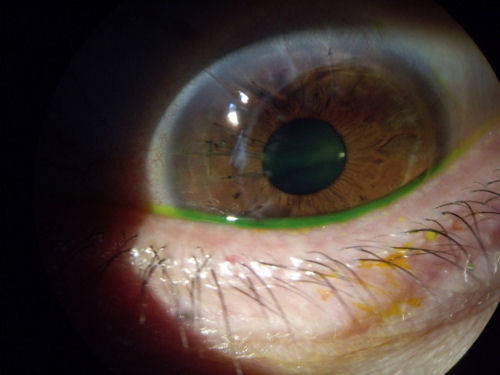
A bad LASIK outcome may result in need for corneal transplant; however, vision may still be poor after the transplant surgery requiring use of hard (rigid) contact lenses. The photo below shows a scleral contact lens over a corneal transplant. You can clearly see the ring around the edge of the donor tissue where the scar formed, bonding the transplant to the cornea.


The image below is a cross sectional scan of a corneal transplant. The patient is wearing a rigid scleral contact lens. The patient had a corneal transplant 10 years ago, which left the patient with poor vision and unable to tolerate any type of corrective lens. With the scleral lens the patient has 20/30 vision and good comfort. Yellow arrows point to the juncture where donor tissue connects to the patient’s cornea. Click image for larger view.
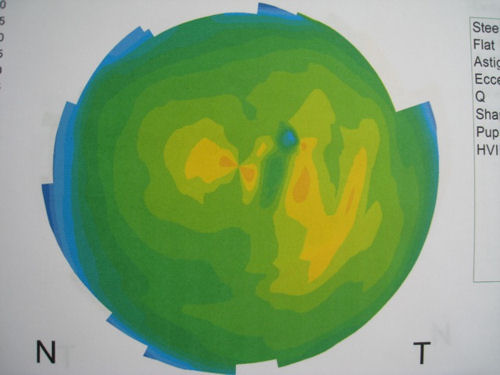
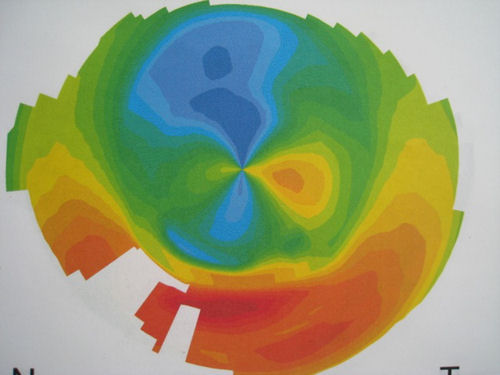
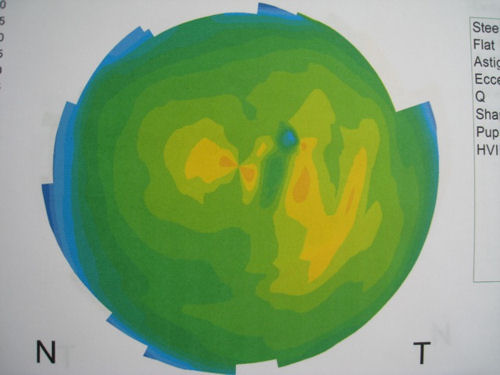
The two images below are corneal topographies of eyes that have undergone corneal transplant. The large range of colors represent significant changes in corneal steepness and refractive power across the central diameter of the cornea. Red represents the steepest areas of the cornea. Deep blue represents the flattest areas. These topographies demonstrate corneas with very irregular surfaces full of hills and valleys and not smooth or spherical. Corneal surface irregularity produces a distorted image on the retina. Compare these topographies of corneal transplants to the topography of a normal eye at bottom.


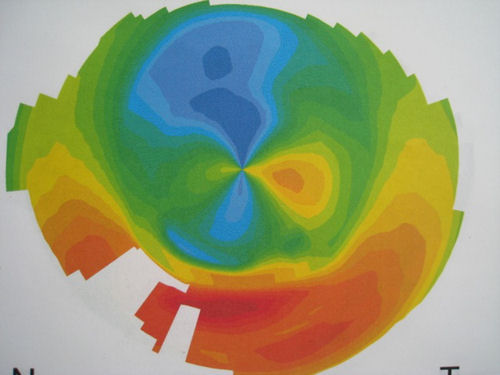
The image below demonstrates a normal unoperated eye with a desirable corneal topography. This patient has normal vision.
Copied by:-http://www.lasikcomplications.com