LASIK permanently thins and weakens the cornea, which may lead to progressive steepening and bulging (ectasia).
LASIK permanently thins and weakens the cornea, which may lead to progressive steepening and bulging (ectasia).Quote: "Ectatic changes can occur as early as 1 week after LASIK, or they can be delayed up to several years after the initial procedure. In many cases, [corneal transplant] is eventually performed to manage this complication... The continuously growing popularity of refractive surgery procedures, namely LASIK, has caused increased concern regarding the serious complication of keratectasia." (Meghpara et al, 2008)
Persons experiencing post-LASIK ectasia or other eye problems should seek the advice of a physician. If you would like to share your story with us, email lasikcomplications(at)yahoo(dot)com or use the contact form located on the menu bar above. Due to the failure of LASIK surgeons to report LASIK complications as required by federal law, it's important that patients who experience ectasia after LASIK file a MedWatch report with the FDA.
In an apparent attempt to hide the truth about post-LASIK ectasia, LASIK surgeons may deliberately misdiagnose post-LASIK corneal ectasia as post-LASIK keratoconus. Keratoconus is a naturally occuring disorder of the cornea which usually affects both eyes and typically begins during puberty or late teen years. If a patient did not have keratoconus or early signs of keratoconus before LASIK, and experienced steepening of the cornea with vision loss after LASIK, then the correct diagnosis is likely ectasia.
On 3/17/2010, a class-action lawsuit was brought against TLC LASIK Centers for allegedly performing LASIK on patients who had pre-existing risk factors for post-LASIK ectasia. Read article; Read lawsuit; Watch videoImages courtesy of Dr. Edward Boshnick, who has devoted his practice to the restoration of quality vision and information on post-LASIK ectasia.
Photos of post-LASIK ectatic corneas
The image below on the left is a photo of a patient who had LASIK in 1997. He developed corneal ectasia (bulging) and started losing his vision several years later. The image below on the right shows the protrusion of a cornea which developed post-LASIK ectasia. The abnormal corneal curvature results in severe visual distortion which is not correctable with glasses or soft contact lenses.


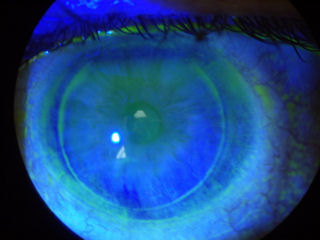
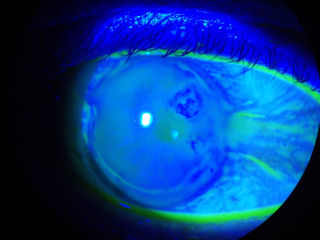
The image below on the left shows a cornea with post-LASIK ectasia treated with INTACS. The patient had LASIK in 2000 and developed ectasia 2 years later. INTACS were inserted in 2006 in an unsuccessful attempt to smooth out the corneal surface. In 2007 white blood cells and protein materials began adhering to the medial aspect of the plastic inserts. The INTACS are at the anterior corneal surface causing the patient discomfort and increased visual aberrations.
Corneal ectasia can occur after Radial Keratotomy (RK) as well as after LASIK. The image below on the right shows the cornea of a patient with post-RK ectasia. The patient had RK in 1988. He began losing visual quality in 1990. In addition to the corneal protrusion, note the faint white spot at the apex of the curve. This is internal corneal tissue that is protruding out of one of the RK incisions.


The photo below on the left is a cornea 8 years after LASIK. The patient developed ectasia. In the photo, you can see that the dye instilled in the eye is staining at the flap-cornea interface -- a clear sign that the LASIK flap-wound is not healed.
The photo below-right shows the eye of a patient who had botched RK surgery followed by a corneal transplant. The transplanted cornea developed ectasia.

The patient in the photo below-left has keratoconus, not post-LASIK ectasia. The patient was implanted with one INTACS, which failed to restore functional vision. The INTACS created a new set of problems, and the patient decided to have it removed. Currently the patient is attempting to wear lenses again, but as you can see, the lens is riding off center. You can also see a suture at the 11:00 position that remains after removal of the INTACS. Also note 3 white scars perpendicular to the suture. Click on image for a larger view.
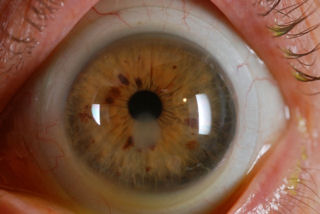
The patient in the photo below-right underwent LASIK in 2000. The dark round area at 2:00 o'clock is the area of the cornea with ectasia. The area is dark due to the elevated irregular surface. For unknown reasons the tear film cannot adhere to the corneal surface where it is bulging, hence, it is much darker than the surrounding corneal tissue. The LASIK flap margin is also clearly visible.
 Iatrogenic keratectasia / ectasia is one of the most feared and dreaded complications of LASIK. The rate of ectasia after LASIK is estimated to be about one in 2,000, but this number could be an underestimate due to underreporting and lack of long-term followup after LASIK. There are likely several thousand patients suffering from post-LASIK ectasia in the United States. The medical literature contains reports of late onset ectasia occuring several years after LASIK.
Iatrogenic keratectasia / ectasia is one of the most feared and dreaded complications of LASIK. The rate of ectasia after LASIK is estimated to be about one in 2,000, but this number could be an underestimate due to underreporting and lack of long-term followup after LASIK. There are likely several thousand patients suffering from post-LASIK ectasia in the United States. The medical literature contains reports of late onset ectasia occuring several years after LASIK. Reported risk factors for ectasia after LASIK include abnormal corneal topography, pre-existing keratoconus, forme fruste keratoconus, or pellucid marginal degeneration (PMD), insufficient stromal bed thickness, high myopia, and age younger than 25 years. Operating on patients with pre-op thin corneas should be avoided.
There is no cure for ectasia. Reported treatments for the management of post-LASIK ectasia include hard contact lenses; intraocular pressure-lowering drugs; and intracorneal ring segments, or INTACS. Frequently, a corneal transplant is required. Corneal collagen cross-linking (CXL or C3R), is a relatively new, experimental treatment for ectasia using riboflavin and UVA light. Learn about clinical trials for treating corneal ectasia with corneal collagen cross-linking at ClinicalTrials.gov: NCT01024322, NCT01112072, NCT01152541, NCT01024322, and NCT01081561.
A 2009 survey of LASIK surgeons found that 37% of respondents have had one or more documented cases of post-LASIK ectasia in his or her surgical patients. (Source: Duffey RJ, Leaming D. US Trends in Refractive Surgery: 2009 ASCRS Survey. Available at: http://www.duffeylaser.com/physicians_resources.php. Accessed April 29, 2010.)
LASIK surgeons have developed a private database of post-LASIK ectasia cases. Here is a link to the members-only online registry. http://www.ectasiaregistry.com/
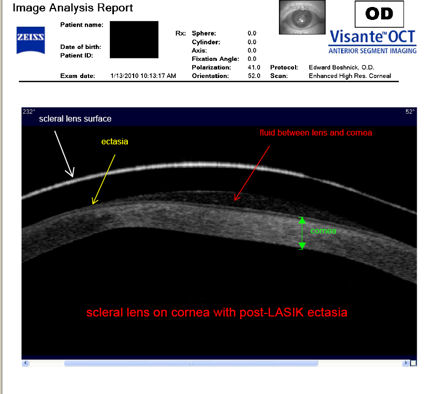
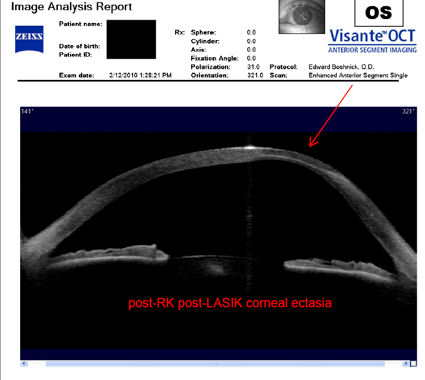
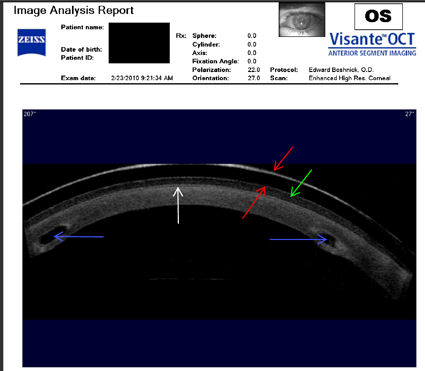
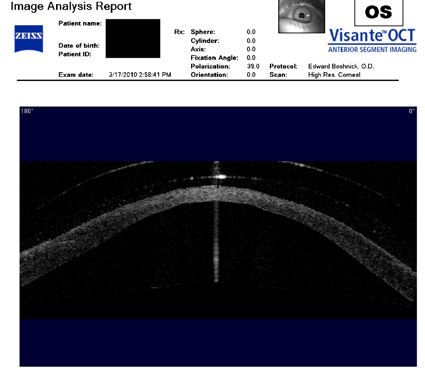
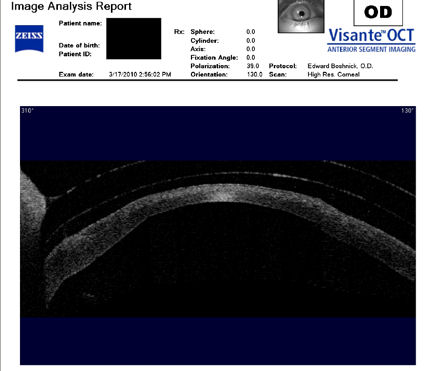
Scans of post-LASIK ectatic corneas
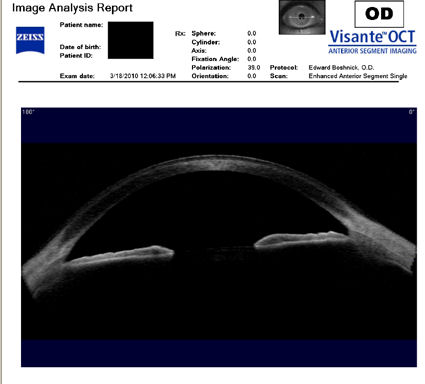
The following images were acquired using a technique called optical coherence tomography, or OCT. The instrument produces a cross-sectional image by scanning the front of the eye (anterior segment) with a beam of light. Think of it like an ultrasound using light instead of sound waves to create an image of living tissues. The image directly below is a scan of a healthy, unoperated cornea for comparison with the following images of post-LASIK ectatic corneas.
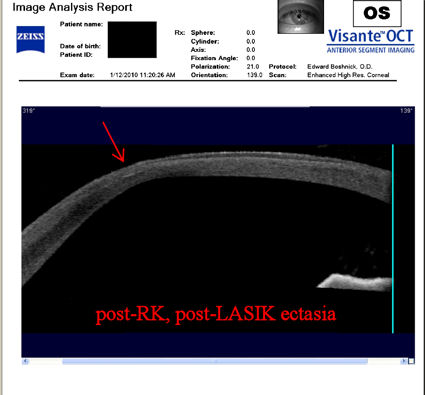
The cornea shown below had RK followed by LASIK and developed corneal ectasia. Click on the image for a larger view.
The next two scans below show a rigid scleral contact lens on a post-LASIK ectatic cornea.

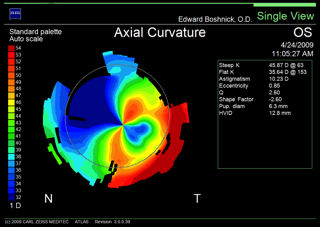
Topographies of post-LASIK ectatic corneas
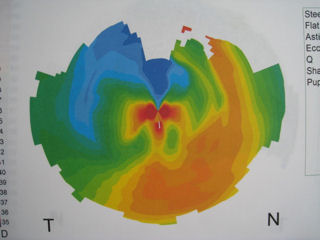
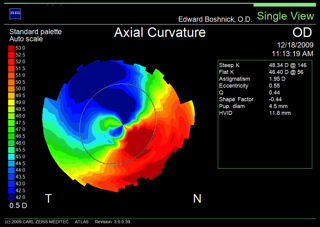
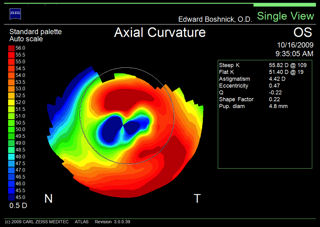
The first three images below are corneal topographies of eyes that developed ectasia after LASIK. The large range of colors represent significant changes in corneal steepness and refractive power across the central diameter of the cornea. Red represents the steepest areas of the cornea where the cornea is protruding. Deep blue represents the flattest areas. These topographies demonstrate corneas with very irregular surfaces full of hills and valleys and not smooth or spherical. Corneal surface irregularity produces a distorted image on the retina. Compare these topographies of post-LASIK ectasia to the topography of a normal, unoperated eye (bottom-right). 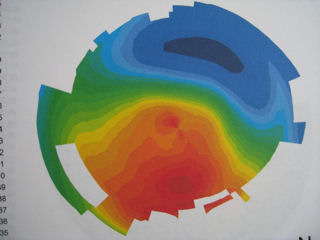
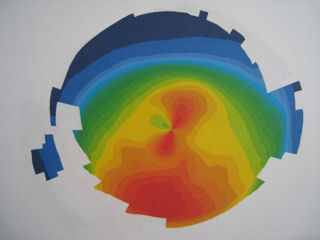

The topography below-left of a post-LASIK eye with ectasia shows extreme power changes within the patient's visual field (central cornea), which leads to severe visual distortions. The deep red area at the 4:00 position is the location of the ectasia (bulging).
The topography below-right shows the steepest area of the cornea (ectasia) at the 11:00 - 12:00 position.
Case reports of post-LASIK ectasia
The photo below-left is a post-LASIK ectatic cornea with hydrops. Progressive bulging and thinning of the cornea associated with ectasia may rarely lead to rupture of the membrane on the back surface of the cornea in response to intraocular pressure, which is known as hydrops. In this case, the patient had LASIK in 2000. Two years later he developed ectasia. In August, 2009 he awoke to a red, cloudy cornea. The back surface of the weakened cornea had ruptured (hydrops), and aqueous fluid from inside the eye entered the cornea, causing this red, cloudy condition. At the time this photo was taken, the patient had no functional vision and could only count fingers at a 12-inch distance. The image to the right of the photograph is a cross-sectional scan of the patient's cornea taken at a later date after the patient underwent a corrective procedure. The two red arrows point to the break on the back surface of the cornea. (The vertical beam of light is an artifact). Click on the scan to enlarge.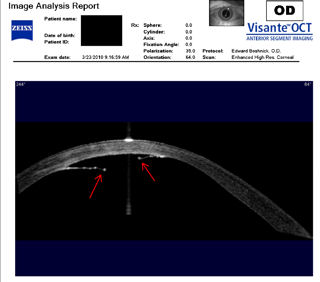 The next two images are photos of an eye that developed ectasia following RK surgery and subsequent LASIK surgery. The image on the left shows the protrusion of the cornea. The image on the right shows the patient wearing a scleral contact lens. The hazy spot at the bottom of the pupil is a scar caused by a laser procedure, which was performed in an unsuccessful attempt to correct the problems caused by the previous surgeries. We call this the "domino effect of unnecessary eye surgery".
The next two images are photos of an eye that developed ectasia following RK surgery and subsequent LASIK surgery. The image on the left shows the protrusion of the cornea. The image on the right shows the patient wearing a scleral contact lens. The hazy spot at the bottom of the pupil is a scar caused by a laser procedure, which was performed in an unsuccessful attempt to correct the problems caused by the previous surgeries. We call this the "domino effect of unnecessary eye surgery".

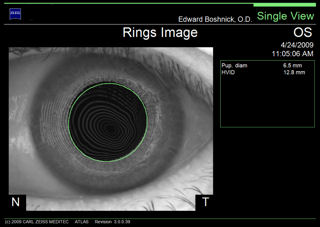
The next three images are the left eye (OS) of a surgeon from Venezuela who had LASIK about 4 years ago and later developed ectasia. He was unable to perform surgery until he was fitted with a special scleral lens. The first two images were acquired with a corneal topographer. In the image labeled "Axial Curvature", the extreme range of colors represent severe irregular astigmatism and significant corneal power changes across the central cornea, which results in severe visual distortions. The image labeled "Rings Image" is a reflection of light from the surface of the eye. In a normal eye, the rings would be perfectly round concentric circles. Click on the image to enlarge and you will see that the rings are irregular and distorted, which indicates that the patient's vision is distorted. The third image, which was taken 10 months later, is a cross-sectional scan of the cornea. The red arrow points to the ectatic area of the cornea.